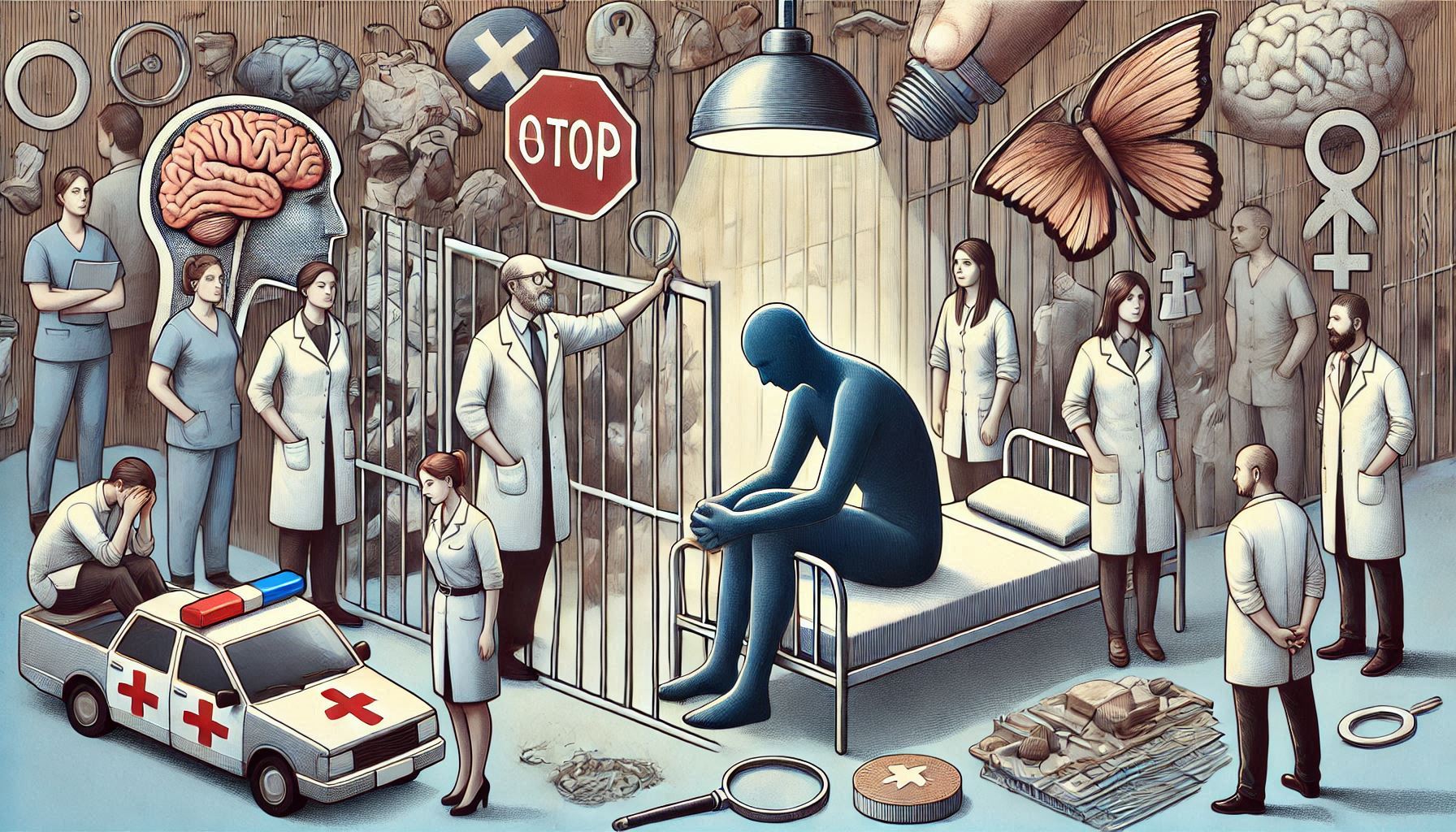
Mental health treatment is an essential part of maintaining well-being, yet millions of people around the world face significant barriers when trying to access care. One of the most profound and pervasive barriers is stigma. Mental health stigma refers to the negative attitudes, discrimination, and stereotypes that affect individuals who experience mental health disorders. These prejudices can prevent individuals from seeking the care they need and contribute to long-term suffering, isolation, and societal exclusion.
What makes stigma even more complex is the intersection of gender. The stigma surrounding mental health issues is not experienced equally by all people—gender plays a substantial role in shaping how individuals perceive their mental health struggles and how they are treated by others. For both men and women, gender-based expectations can create unique challenges in terms of acknowledging mental health concerns and seeking help. The consequences are profound and wide-ranging, affecting not only the individuals experiencing mental health challenges but also families, communities, and society as a whole.
This guide explores the connection between stigma and gender as a barrier to mental health treatment. It will address how gender shapes the experience of mental illness, the societal expectations that fuel stigma, and the unique challenges faced by different genders when it comes to seeking and receiving mental health care. The goal is to provide an in-depth understanding of how these factors interact and what can be done to reduce stigma and improve mental health care for all genders.
Understanding Mental Health Stigma
Before delving into the intersection of stigma and gender, it is important to understand what mental health stigma is and how it operates in society. Mental health stigma can be categorized into two broad types: public stigma and self-stigma.
Public Stigma
Public stigma refers to the societal attitudes, beliefs, and stereotypes that lead to discrimination and negative perceptions of people with mental health conditions. This kind of stigma is shaped by cultural norms, societal values, and media representations, and it can manifest in overt or subtle forms. For example, someone with depression might be perceived as lazy or weak, while someone with anxiety may be considered overly nervous or irrational. These stereotypes often lead to social exclusion, making it harder for individuals to live fulfilling, connected lives.
The stigma surrounding mental health has deep historical roots, and for centuries, people with mental health conditions were treated as outcasts or even criminals. Although attitudes have improved in many parts of the world, mental health stigma remains pervasive today. Public stigma is reinforced by negative portrayals of mental health in media and by a lack of education about mental illness. Furthermore, mental health conditions are often misunderstood, and people with these conditions are sometimes blamed for their struggles.
Self-Stigma
Self-stigma, on the other hand, occurs when individuals internalize the negative societal beliefs and judgments about mental health. This can lead to feelings of shame, guilt, or unworthiness. People with mental health conditions may feel as though they are not deserving of help or may avoid seeking treatment because they fear being judged by others. The internalization of stigma can result in increased isolation, decreased self-esteem, and a reluctance to talk about mental health issues openly.
Both public and self-stigma are powerful forces that can deter people from seeking mental health treatment, leading to untreated conditions and deteriorating well-being. These forms of stigma often prevent individuals from addressing their emotional and psychological needs, which can exacerbate the mental health crisis globally.
The Role of Gender in Mental Health Stigma
Gender influences how mental health is perceived, experienced, and treated. While mental health issues can affect anyone, regardless of gender, the stigma surrounding these issues can manifest in different ways for men and women due to societal expectations, traditional gender roles, and cultural norms. These gendered expectations not only influence the types of mental health conditions that are most commonly diagnosed in each gender but also affect how individuals of different genders seek help and how their struggles are understood.
Gendered Expectations and Mental Health
Gendered expectations dictate how individuals are expected to behave based on their sex. These expectations can be harmful, especially when it comes to mental health. For example, men are often expected to be strong, independent, and unemotional. These ideals of masculinity create immense pressure for men to suppress their emotions and avoid expressing vulnerability. As a result, men may be less likely to seek help for mental health issues, even when they are experiencing significant distress.
In contrast, women are often expected to be nurturing, emotionally expressive, and attuned to the needs of others. While these traits are seen as positive in many contexts, they can also contribute to an imbalance when women experience mental health challenges. Women are more likely to be diagnosed with depression, anxiety, and other mental health conditions, but their concerns may be dismissed or trivialized as being “overly emotional” or “hormonal.” This gendered perception of women’s emotional struggles can lead to inadequate treatment or misdiagnosis.
At the same time, both men and women face challenges that are uniquely tied to their gender. For men, the pressure to conform to traditional masculinity can make it difficult to acknowledge mental health challenges, while for women, societal expectations regarding emotional expression and caregiving roles may lead to greater vulnerability to certain mental health conditions. These gendered experiences shape how individuals perceive their mental health struggles and how they are likely to seek or avoid treatment.
Stigma and Men’s Mental Health
The Masculine Ideal: Strength and Stoicism
Historically, the concept of masculinity has been tied to strength, self-reliance, and stoicism. Men are often expected to handle their emotions privately and to be in control of their feelings, which creates an environment where seeking help for mental health issues is viewed as a sign of weakness. This expectation that men must always be tough and unflinching leads many to internalize the belief that they should be able to “handle it” on their own.
As a result, mental health conditions such as depression, anxiety, and emotional distress may go unaddressed in men, as they avoid seeking help due to fear of being seen as weak or vulnerable. Research has consistently shown that men are less likely than women to seek professional help for mental health issues, even when they exhibit similar symptoms. For instance, a study by the American Psychological Association found that men were less likely to seek mental health services even when experiencing significant symptoms of depression.
Coping Mechanisms: Risky Behaviors and Substance Abuse
Instead of seeking professional help, many men may turn to unhealthy coping mechanisms such as substance abuse, anger, or violence. These behaviors are often seen as more socially acceptable expressions of emotional distress for men, as they align with societal expectations of masculinity. Substance abuse, in particular, is a common way for men to cope with feelings of isolation, sadness, or anxiety without appearing emotionally vulnerable.
Unfortunately, these maladaptive coping strategies only exacerbate mental health issues. Substance abuse and other risky behaviors often lead to additional health problems, social issues, and complications that further hinder a man’s ability to address the root causes of their mental health struggles.
Men’s Mental Health Diagnosis and Treatment
When men do seek help, there is evidence to suggest that mental health professionals may not always take their symptoms seriously. Men are less likely to be diagnosed with depression or anxiety, even when these disorders are clearly present. This underdiagnosis is partially due to the fact that men often present with mental health issues differently than women. For example, men may exhibit more irritability, anger, or aggression when experiencing depression, which may lead healthcare providers to miss the underlying cause of these behaviors.
In some cases, mental health professionals may dismiss men’s emotional struggles as “normal” or “expected” for their gender. This creates a cycle in which men feel discouraged from seeking help or receiving the proper treatment, leading to worsening mental health issues.
Stigma and Women’s Mental Health
The Emotional Labor of Womanhood
For women, the stigma surrounding mental health is closely tied to societal expectations of emotional labor and caregiving. Women are often expected to prioritize the needs of others over their own, and this expectation can be emotionally draining. When women experience mental health issues, they may be reluctant to seek help, fearing that they will be seen as failing to meet their roles as wives, mothers, or caregivers.
Women are often diagnosed with depression and anxiety more frequently than men, and this diagnosis is sometimes attributed to hormonal fluctuations, relationship difficulties, or caregiving stress. These explanations can diminish the validity of women’s emotional distress and lead to treatment approaches that fail to address the underlying causes of their mental health struggles. Additionally, women are often labeled as “overly emotional” or “hysterical” when expressing feelings of sadness or anxiety, which can reinforce their reluctance to seek help.
The Impact of Gendered Trauma
Many women experience gender-based violence, including sexual assault, domestic violence, and harassment, which can have long-lasting psychological effects. These experiences of trauma are often dismissed or minimized, especially if the woman is perceived as “too emotional” or “unstable.” Gendered trauma, particularly sexual violence, can contribute to mental health conditions such as post-traumatic stress disorder (PTSD), depression, and anxiety.
However, societal attitudes toward gendered trauma can lead to the stigmatization of women who have experienced such violence. They may be blamed for their victimization, or their emotional responses may be seen as an overreaction rather than a legitimate mental health issue.
Intersectionality: Race, Class, and Gender
For women of color, the stigma surrounding mental health is compounded by the intersections of race, class, and gender. Women from marginalized communities face unique challenges when it comes to mental health, including racial discrimination, economic inequality, and cultural barriers to accessing care. These women are less likely to seek mental health services and more likely to experience negative outcomes when they do.
For example, Black women may face both racial and gender-based discrimination in healthcare settings, leading to misdiagnosis, underdiagnosis, and unequal treatment. The compounded effects of racism and sexism create additional layers of stigma that can prevent these women from seeking or receiving the mental health care they need.
How Stigma Creates Barriers to Treatment
The stigma surrounding mental health is a significant barrier to treatment for both men and women. Gendered expectations can shape not only the internalized stigma individuals feel but also the external stigma they encounter in their communities, workplaces, and healthcare systems.
Reluctance to Seek Help
The fear of being judged or misunderstood can prevent individuals from reaching out for help. Men, fearing that seeking treatment will make them appear weak, may avoid therapy or counseling. Similarly, women who fear being labeled as “overly emotional” or “irrational” may hesitate to discuss their mental health concerns with family members, friends, or healthcare providers.
This reluctance to seek help is compounded by the lack of gender-sensitive mental health services. Healthcare providers who are not trained to recognize how gender influences mental health may inadvertently reinforce gender stereotypes, making it even harder for individuals to feel comfortable disclosing their concerns. For instance, male patients may feel dismissed if their emotional struggles are minimized or labeled as “normal” for men, while female patients may feel unheard if their emotional experiences are attributed to hormonal imbalances or a failure to meet societal expectations of womanhood.
Impact on Treatment Outcomes
When individuals do seek treatment, gender-related stigma can affect the quality of care they receive. Healthcare providers may unconsciously harbor biases based on gender norms, leading to inaccurate diagnoses or treatment plans that do not fully address the individual’s needs.
For example, a male patient presenting with symptoms of depression may be misdiagnosed with a personality disorder or substance abuse issue, rather than being treated for depression. A female patient, on the other hand, may be prescribed medication for anxiety without exploring the root causes of her symptoms, which may be linked to societal pressures or past trauma.
Furthermore, the stigma associated with seeking treatment can cause individuals to prematurely disengage from therapy or medication, especially if they do not feel validated or supported. Without ongoing treatment, mental health conditions can worsen, leading to further complications and a cycle of untreated illness.
Gender and Mental Health Treatment: Barriers and Solutions
The barriers created by gendered stigma are significant, but they are not insurmountable. To reduce stigma and increase access to mental health care, society must address the underlying cultural norms and stereotypes that perpetuate gendered stigma. The following strategies can help create a more supportive environment for all individuals, regardless of gender:
Education and Awareness
Public education campaigns can help challenge and redefine traditional gender norms related to mental health. By highlighting the importance of emotional health and encouraging both men and women to seek help, these campaigns can normalize mental health care. Awareness campaigns should also educate the public about the unique ways in which mental health issues affect men and women and the importance of removing gender-based barriers to treatment.
Gender-Sensitive Mental Health Care
Healthcare providers must receive training on how gender influences the experience of mental health issues. Mental health professionals should understand that men and women may present symptoms differently and that cultural and gender-based biases can affect diagnoses. Gender-sensitive care should be offered, ensuring that individuals of all genders feel seen and understood in their treatment.
Creating Safe Spaces for Discussion
Creating safe, supportive spaces for people to talk about their mental health challenges is crucial in reducing stigma. These spaces should be welcoming to individuals of all genders and should acknowledge the unique challenges that different genders face. Support groups, online communities, and peer networks can be effective tools in breaking down the silence and isolation surrounding mental health.
Breaking the Silence
Finally, breaking the silence surrounding mental health is essential. Conversations about mental health must be normalized in homes, schools, workplaces, and communities. Open dialogue about mental health, especially among men and women, can help to deconstruct harmful stereotypes and promote a more empathetic approach to mental illness.
Conclusion
Stigma surrounding mental health is a major obstacle to treatment for individuals of all genders. Societal norms and gender expectations significantly influence how people experience mental health challenges and how they are perceived when seeking help. These gendered pressures often lead to different experiences for men and women, shaping both the nature of the mental health issues they face and how these issues are addressed. For example, men may be discouraged from expressing vulnerability due to societal expectations of strength and emotional stoicism, while women may face dismissal of their emotional struggles as “overly emotional” or a result of hormonal fluctuations. To overcome these barriers, a comprehensive and inclusive approach is necessary. Mental health initiatives must acknowledge the diverse ways gender impacts mental health and strive to reduce stereotypes associated with mental health struggles. This can be achieved by creating awareness campaigns that challenge traditional gender norms and promote the understanding that mental health issues can affect anyone, regardless of gender. Moreover, it’s vital to provide gender-sensitive mental health care that addresses the specific needs of different groups while fostering an environment that encourages all individuals to seek help without fear of judgment. By breaking down the gendered stigma surrounding mental health, society can empower individuals to reach out for the support they need. When people feel understood and supported in their mental health journey, treatment becomes more accessible, effective, and impactful. Ultimately, dismantling the barriers created by gender-based stigma can lead to a more inclusive and compassionate mental health care system that serves everyone equally, improving overall well-being and quality of life for individuals across all genders.
SOURCES
Corrigan, P. W. (2016). Stigma and mental illness: A review of the literature. Journal of Social and Clinical Psychology, 35, 539-565.
Addis, M. E. (2008). Gender and depression in men. Clinical Psychology: Science and Practice, 15(3), 153-168.
Mahalik, J. R., Burns, S. M., & Syzdek, M. (2007). Masculinity and perceived normative health behaviors as predictors of men’s health behaviors. Social Science & Medicine, 64(11), 2201-2209.
Rosenfield, S., & Mouzon, D. M. (2013). Gender and mental health: Do women have more depression, or do they just get more depressed? Gender & Society, 27(6), 838-861.
Kuehner, C. (2017). Why is depression more common among women than among men? The Lancet Psychiatry, 4(2), 146-158.
Vogel, D. L., Wade, N. G., & Haake, S. (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53(3), 325-337.
Hammond, W. P. (2012). Black mental health and mental illness stigma: The role of race-related stress. The Journal of Black Psychology, 38(2), 219-243.
Rochlen, A. B., McKelley, R. A., & Suizo, M.-A. (2008). A critical review of the role of masculinity in men’s help-seeking for depression. Psychology of Men & Masculinity, 9(3), 151-162.
Blashill, A. J., & Karpinski, R. I. (2012). Masculinity, social dominance orientation, and mental health in men. Psychology of Men & Masculinity, 13(4), 422-431.
González, H. M., Tarraf, W., Whitfield, K. E., & Vega, W. A. (2010). The epidemiology of major depression and ethnicity in the United States. Journal of Psychiatric Research, 44(15), 1043-1051.
West, C., & Zimmerman, D. H. (1987). Doing gender. Gender & Society, 1(2), 125-151.
Wang, P. S., Berglund, P. A., & Olfson, M. (2005). Failure and delay in mental health care in the United States. Archives of General Psychiatry, 62(6), 609-616.
Terman, L. M., & Miles, C. R. (1936). Sex and personality. McGraw-Hill.
HISTORY
Current Version
December 10, 2024
Written By:
SUMMIYAH MAHMOOD







Leave a Reply