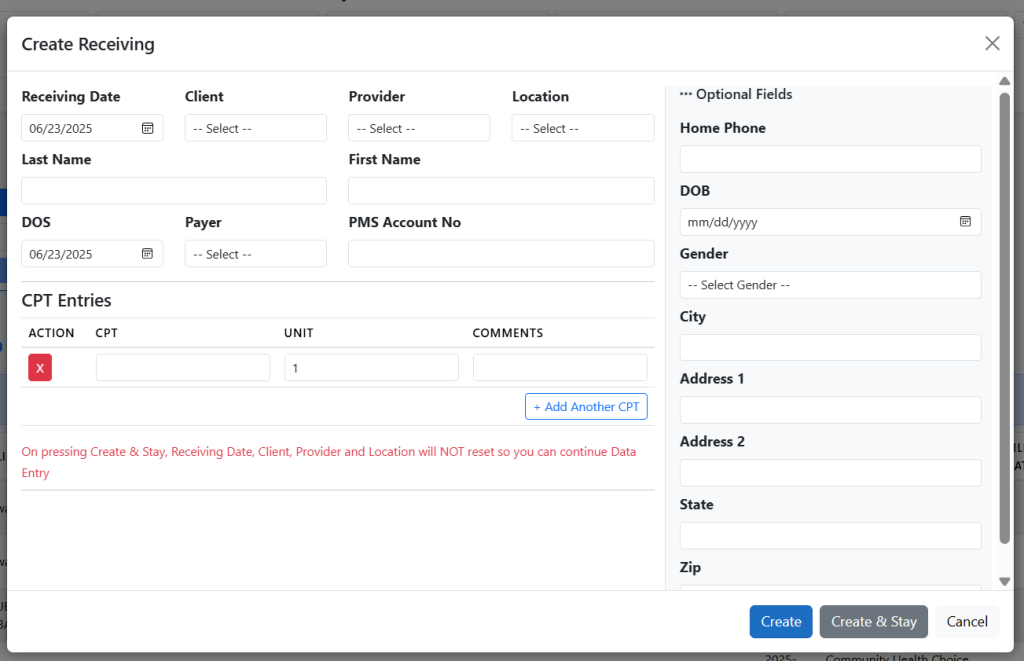
Receiving
Start Strong with Clear Record Intake
Accurate billing begins with accurate data. The Receiving module allows your team to log new patient entries or incoming case files quickly and efficiently. Whether data is entered manually or imported in bulk, the system tracks each entry’s initiation point.
Advanced Filters
Instantly sort records by Receiving Date, Date of Service (DOS), Client, Provider, Location, and more — making it easy to focus on specific data.
Centralized View
See all newly received cases in one place, with clear statuses and search functionality for efficient handling.
Workflow Trigger Point
Aging and next-step tracking begin only after a record is received, ensuring accurate billing timelines.
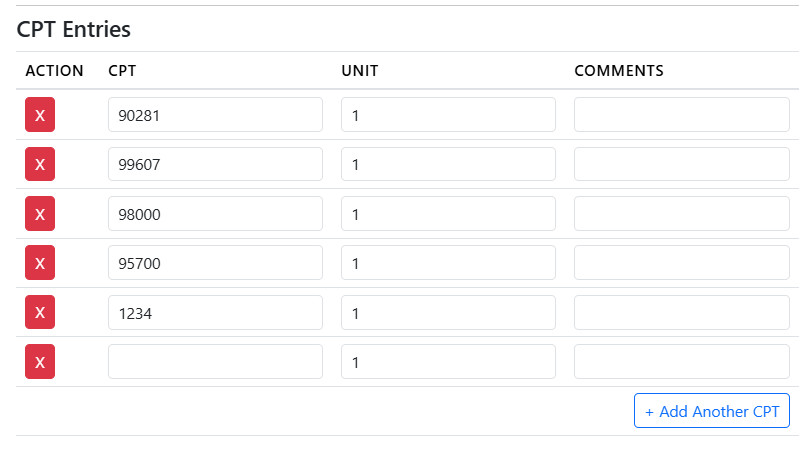
CPT Entry
Add and Manage Procedure Codes with Flexibility
Easily assign multiple CPT codes during the receiving process. The system supports unlimited CPT additions, helping you capture all relevant procedures without limits.
Multiple CPT Support
Easily add one or more CPT codes per entry — no limitations on the number of procedures recorded.
Billing Readiness Tracker
Entries with missing CPTs are clearly flagged, so your team knows exactly what needs attention before billing.
Streamlined Workflow Transition
CPT completion automatically moves entries forward to the billing stage, reducing delays and confusion.
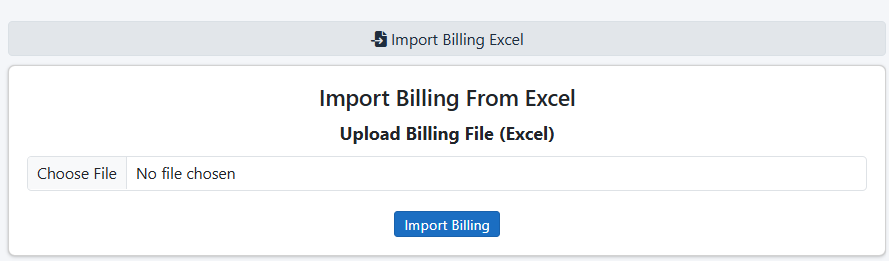
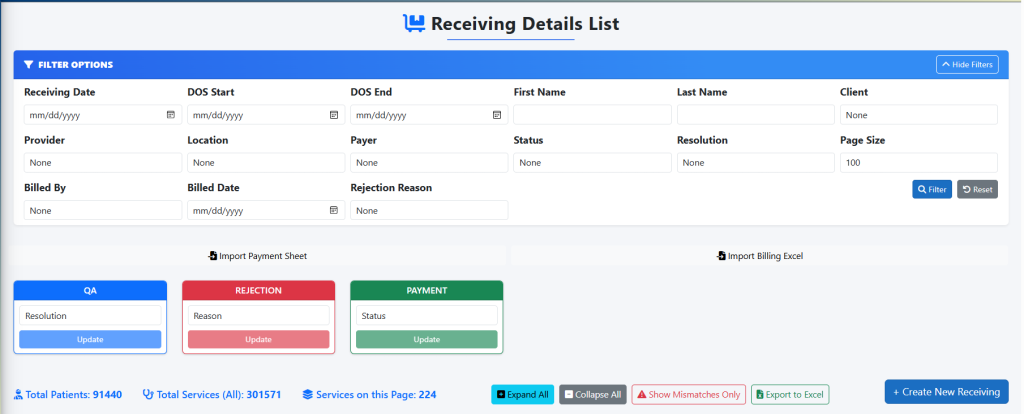
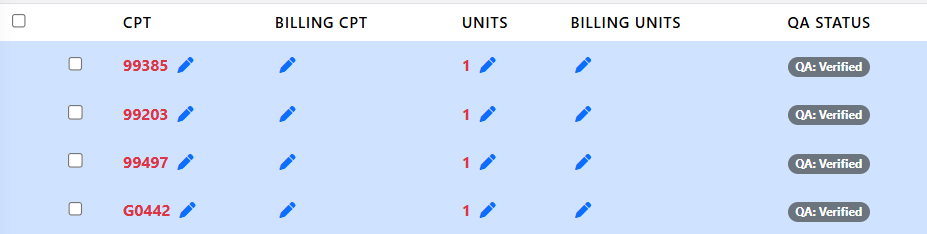
Billing
Automated and Editable Charge Entry
In the Billing stage, billers can import IPA Custom sheets to automatically populate the Billed By and Billed Date fields. Entries can also be reviewed and edited manually within the Billing tab, ensuring flexibility and accuracy before progressing further in the workflow.
IPA Sheet Import
Quickly populate billing details by importing IPA Custom sheets — reducing manual effort and ensuring consistency.
Editable Billing Fields
Manually update or correct Billed By and Billed Date directly from the Billing tab as needed.
Status Visibility
Easily identify entries pending billing and track progress in real time across all records.
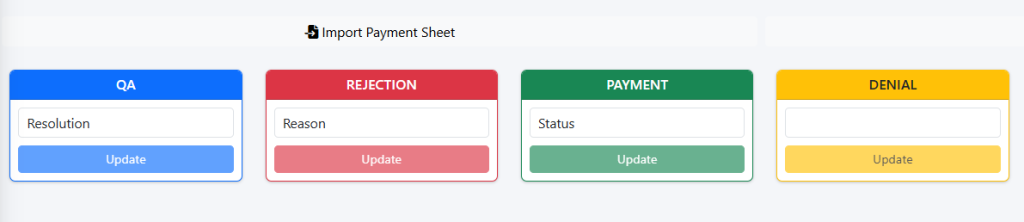
Quality Assurance (QA)
Verify and Validate Before Payment
The QA stage ensures all billing data is accurate before moving forward. Entries are reviewed for completeness, errors, and compliance, helping maintain quality and reducing claim rejections.
Error Prevention
Catch missing or incorrect information before it reaches the payment stage.
Workflow Accuracy
Only QA-approved entries proceed to payment, ensuring clean handoffs.
Team Accountability
Track who completed QA for each entry with built-in user activity logs.
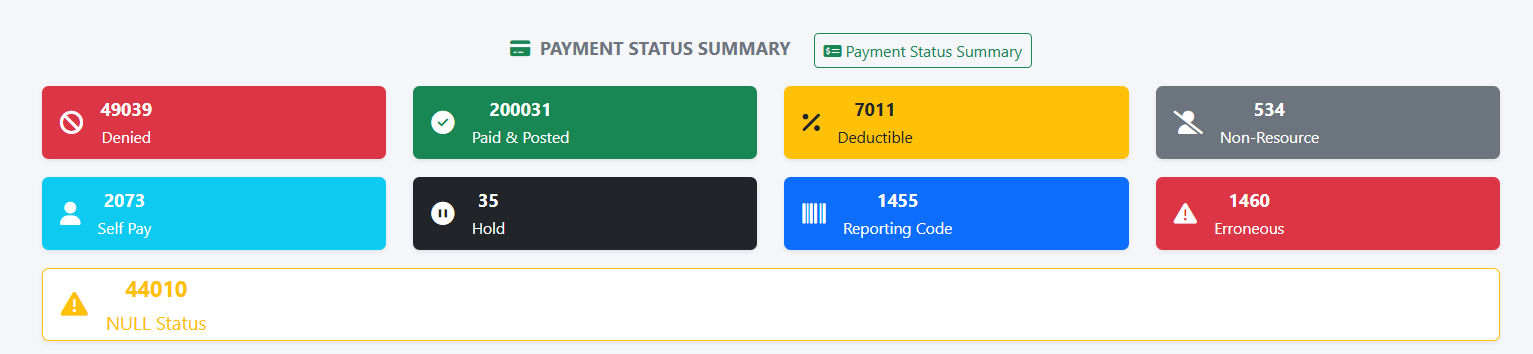
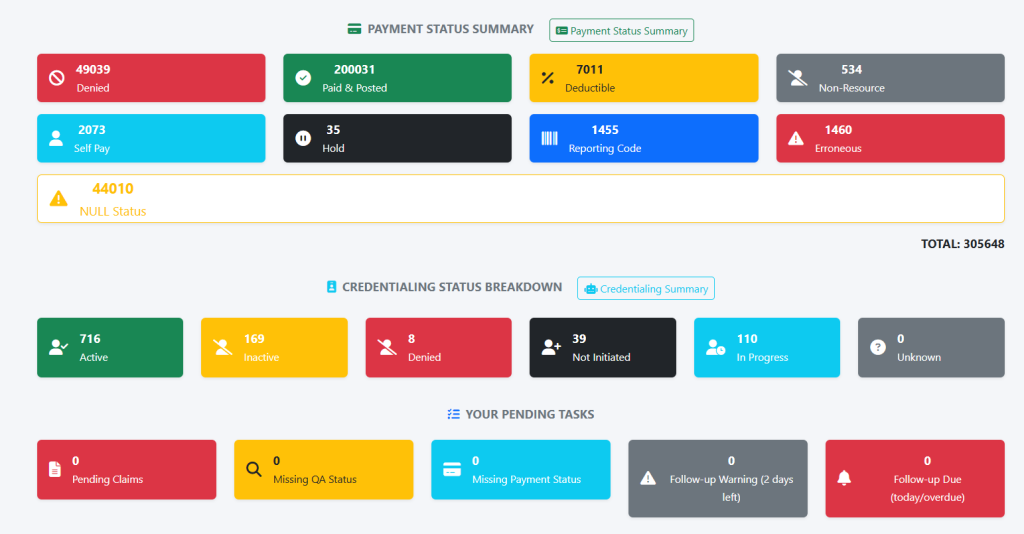
Payment
Track and Post Payments with Confidence
Manage posted and pending payments with clarity. You can post full or partial payments and monitor aging timelines accurately, starting only after the receiving stage is complete.
Payment Tracking
View the status of each entry — paid, partially paid, or pending.
Financial Transparency
Easily track outstanding balances and ensure timely follow-ups.
Aging Control
Aging starts only after receiving, giving you better control over billing timelines.
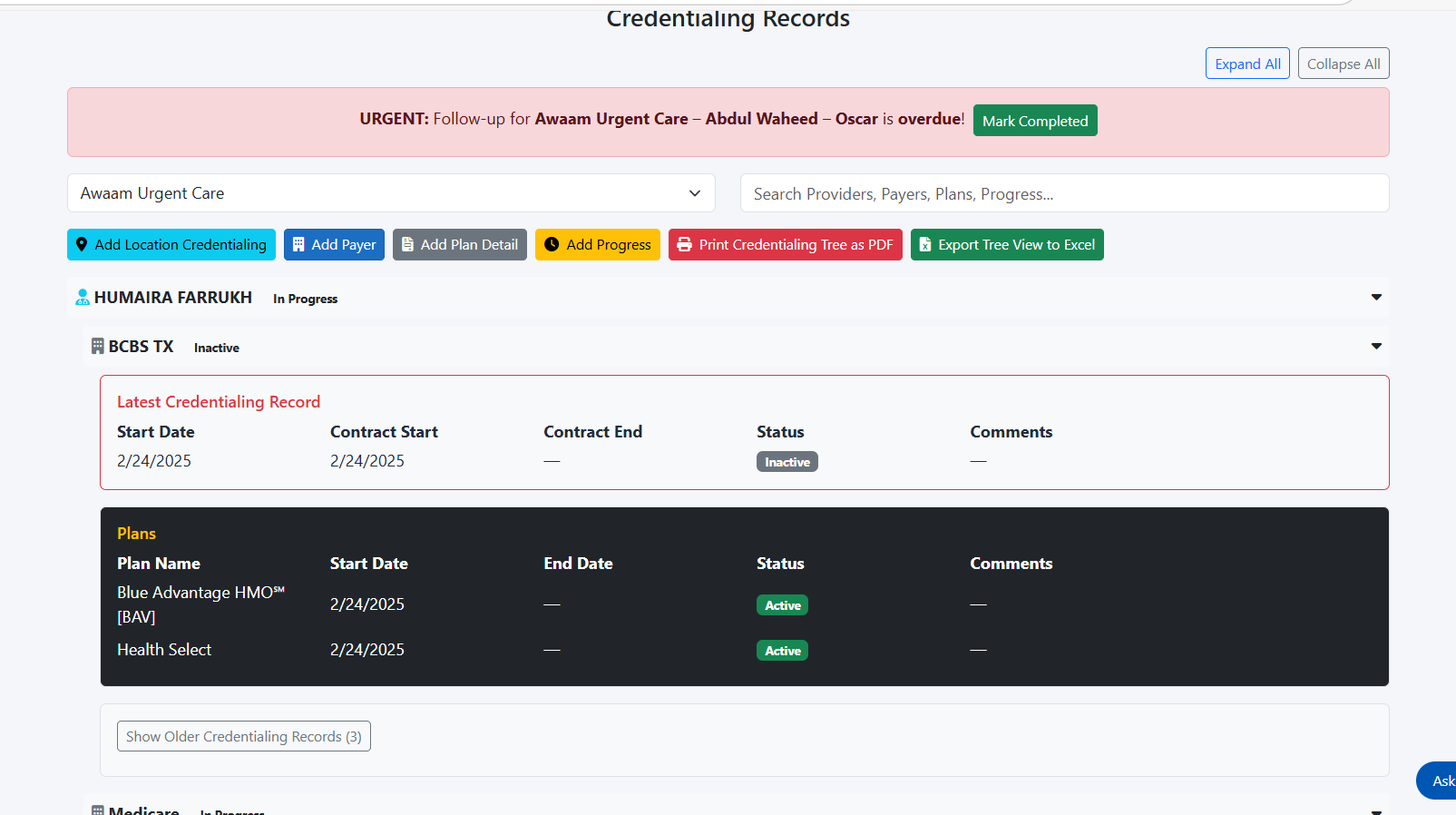
Credentialing
Track Provider Status with Real-Time Alerts
The Credentialing tab helps you manage and monitor provider credentialing workflows with complete transparency. From initial submission to approval, every stage is tracked — and urgent follow-ups are clearly highlighted to avoid delays.
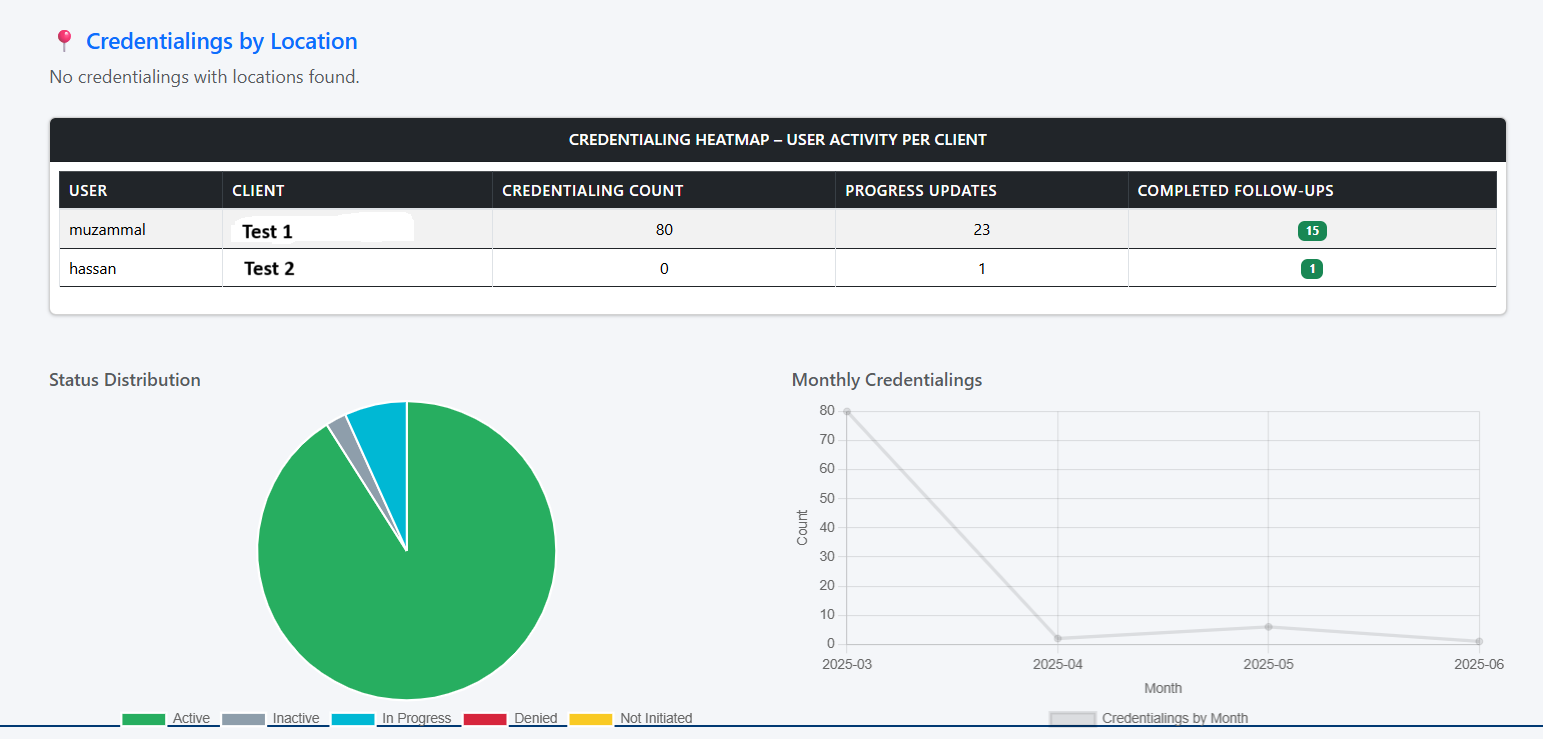
Status Breakdown
View detailed credentialing states such as Active, Inactive, In Progress, Not Initiated, and more — all in one place.
Urgent Follow-Up Alerts
Receive real-time alerts for overdue tasks.
Progress Tracking
Monitor ongoing credentialing efforts across teams and providers with user-wise tracking.
Recent News
Latest Updates and News
-

Remote RCM Teams: Managing Productivity in Virtual Mental Health Billing
In the evolving landscape of healthcare administration, remote Revenue Cycle Management (RCM) teams are no longer an exception but a growing norm—particularly in the field…
-

Building an RCM Leadership Team in Your Behavioral Health Practice
In today’s complex and fast-evolving healthcare environment, behavioral health practices face a unique set of revenue cycle management (RCM) challenges. These include high claim denial…
-
Training Administrative Staff in Mental Health-Specific RCM Protocols
In the rapidly evolving landscape of mental healthcare, the importance of an efficient Revenue Cycle Management (RCM) system cannot be overstated. RCM serves as the…